
By Aaron Allen, The Seattle Medium
A plethora of factors contribute to health disparities affecting the Black community, including trust issues, access to care, poor quality of care, community features such as inadequate access to healthy foods, poverty, limited personal support systems, and violence. Additional factors include genetics, language barriers, health behaviors, and environmental conditions like poor air quality.
Statistics and data highlight the stark reality of health inequity. In the 30 largest American cities, there are more than 74,000 excess deaths among Black people compared with White people each year. This disparity is evident in the prevalence and impact of systemic lupus erythematosus (SLE), or lupus, a chronic autoimmune disease that disproportionately affects the Black community.
Lupus is a chronic (long-term) disease that can cause inflammation and pain in any part of your body. It’s an autoimmune disease, which means that your immune system, the body system that usually fights infections, attacks healthy tissue instead. Lupus most commonly affects your skin, joints, and internal organs, like your kidneys and heart. Because lupus affects many parts of the body, it can cause a lot of different symptoms.
According to the Lupus Foundation of America:
• African Americans have a higher prevalence of lupus than other groups, with rates ranging from 34% to 51%. In comparison, Hispanic patients have a prevalence of 31% to 49%, Asian patients range from 33% to 82%, and White patients have the lowest prevalence at 13% to 23%.
• White patients are more likely to participate in clinical trials, representing as much as 51% of trial participants, whereas Hispanic patients make up 16% of prevalent cases and 21% of trial enrollees, and Asian patients account for 13% of prevalent cases and 10% of trial enrollees.
• Black and Hispanic women with lupus are more likely to die earlier than other groups. Black women with lupus can die up to 13 years earlier than non-Hispanic White women with lupus. Hispanic and Asian women with lupus are 4 to 6 times more likely to die than the general population. Additionally, African American and Hispanic women tend to develop lupus at a younger age and experience more severe symptoms than other groups.
Jawanna Perine suffered from a variety of pains and discomfort from an early age. It wasn’t until her twenties, after countless diagnoses from arthritis to growing pains, that she was diagnosed with lupus.
“I remember being very young and having these muscle and joint pains and going to the doctor and this was before like age 10 and [the doctors] not really knowing what was going on,” says Perine. “Throughout my grade school, middle school, and high school, I wasn’t able to participate in PE, sports, anything because I would have trouble with my legs. But I wasn’t diagnosed with lupus until I was 29, literally months from my 30th birthday.”
“So, all those years prior to that I had pretty much been misdiagnosed,” Perine continued. “It was kind of a bittersweet process because after a while of going to the doctors back and forth and being told that it’s arthritis or this or that and I remember in high school like for years they told me that it was just growing pains.”
According to experts, when people talk about lupus, they’re usually talking about systemic lupus. But there are four kinds of lupus: Systemic lupus erythematosus (SLE), the most common form of lupus; Cutaneous lupus, a form of lupus that is limited to the skin; Drug-induced lupus, a lupus-like disease caused by certain prescription drugs; Neonatal lupus, a rare condition that affects infants of women who have lupus.
Research shows Black patients with SLE are less likely than White patients to receive standard-of-care vaccine recommendations from their physicians, despite higher risks for serious infections and acute care use for vaccine-preventable illnesses. The disproportionate burden of current individuals with SLE accentuates the importance of working to improve avoidable diseases and illnesses.
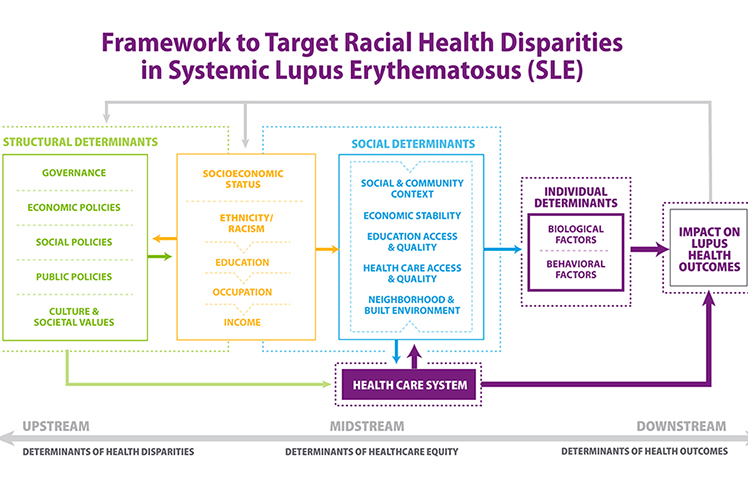
According to a report by the National Institutes of Health (NIH), “Systemic lupus erythematosus (SLE) is a chronic autoimmune disease,” according to the NIH. “The complex relationships between race, ethnicity, and social determinants of health (SDOH) in influencing SLE and its course are increasingly appreciated. Multiple SDOH have been strongly associated with lupus incidence and outcomes and contribute to health disparities in lupus.”
“Measures of socioeconomic status, including economic instability, poverty, unemployment, and food insecurity, as well as features of the neighborhood and built environment, including lack of safe and affordable housing, crime, stress, racial segregation, and discrimination, are associated with race and ethnicity in the US and are risk factors for poor outcomes in lupus,” the NIH report continued.
Linda, a 32-year-old community organizer, discovered she had lupus in January of 2019. Both Linda and Perine were aware of the condition due to its hereditary nature, having witnessed family members endure and succumb to the illness.
“I was kind of devastated. I knew that it could have a real impact,” says Linda after being diagnosed with lupus. “It really impacted my mother and threatened her life a few times. It had been debilitating in different stages of her life. So, I mean I wasn’t happy, I was sad.”
The initial devastation gave way to hope as Linda began her treatment.
“Again, I was pretty devastated for a moment, but I think that kind of went away once I started getting on medication, taking away the initial pain and discomfort that I was experiencing and the sickness that I was experiencing,” says Linda.
Both Linda and Perine emphasize that anyone can develop lupus, but certain groups are at higher risk. This includes women ages 15 to 44, and certain racial or ethnic groups such as African Americans, Asian Americans, Hispanic/Latino individuals, Native Americans, and Pacific Islanders. Lupus is also hereditary, and those with a family member who has lupus or another autoimmune disease are at an increased risk.
“I know that disease does not discriminate,” says Perine. “But for some reason, the medical field measures through the disparities and even though men, women, because disease doesn’t discriminate, everybody is susceptible to lupus. But for some reason, Black people, Latino people, Asian people seem to contract it more than any other.”
Linda shares an important message about self-blame and the need for resilience.
“Don’t blame yourself,” says Linda. “I think there’s a period of time that you go through after diagnosis where you blame yourself, blame your lifestyle, blame things that you’re doing. It can be as simple yet unfortunate as being someone who has inherited this. I know there’s a lot of research that is happening but, it’s part genetics and especially as Black women, it’s also I feel a part epigenetic.”
“So, our long history with trauma and racism and the legacy of enslavement, those things really forced our bodies and our immune systems to work really hard and to overwork. So, really be patient with yourself. Don’t blame yourself and just continue to change and make your life a healthy life and live every day,” she concluded.