Nigeria’s already fragile healthcare system is facing a critical manpower deficit, as the number of licensed doctors has dropped to about 40,000, far below the estimated 300,000 needed to adequately serve a population of over 220 million, PUNCH HealthWise can authoritatively report.
In 2024, the Minister of Health and Social Welfare, Prof. Muhammad Pate, revealed that Nigeria had about 55,000 licensed doctors.
Speaking during an interview on Channels TV’s Politics Today, Pate disclosed that no fewer than 16,000 doctors had left the country in the past five years, while about 17,000 others had been transferred out of active service.
READ ALSO: 20 Winners Emerge In Governor Otu Project Trivia Writing Challenge, Get Credit Alerts
Worrisomely, a new revelation by the Lagos State Commissioner for Health, Prof. Akin Abayomi, indicates that the number of practising doctors in Nigeria has declined from 55,000 to 40,000 within just one year.
In his presentation at a one-day leadership dialogue in Lagos themed “Strengthening PHC Systems: A Joint Leadership Dialogue,” Abayomi identified manpower shortage as one of the most critical challenges facing the health sector.
The dialogue, organised by the Lagos State Primary Health Care Board with support from development partners, addressed barriers hindering PHCs from meeting expectations and proposed practical solutions for building sustainable PHCs with lasting impact.
Abayomi stated that Lagos currently has only 7,000 doctors serving an estimated 30 million residents, far below the number needed for optimal care delivery.
The commissioner raised concerns over the acute shortage of health workers in the state, disclosing that the state requires an additional 33,000 doctors to meet the healthcare demands of its growing population.
“Nigeria currently has about 40,000 doctors against an estimated need of 300,000, while Lagos alone requires about 33,000 doctors but has only about 7,000,” he said.
According to him, Lagos’ doctor-to-population ratio remains far below what is required for optimal healthcare delivery, noting that the state’s doctors are serving an estimated population of nearly 30 million people.
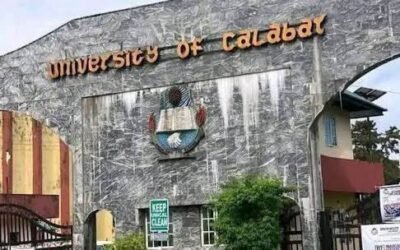
To address the shortfall, Abayomi said the state government is investing in its newly established University of Medicine and Health.
“Within five years, UMH will produce about 2,500 healthcare workers annually, including laboratory scientists and other essential cadres,” he stated.
The mass exodus of healthcare professionals popularly known as japa syndrome, especially doctors, nurses, and pharmacists has remained a major concern in Nigeria.
A 2017 survey conducted by a Nigerian polling organisation in partnership with Nigeria Health Watch revealed that about 88 per cent of Nigerian doctors were seeking job opportunities abroad at the time.
Healthcare leaders have attributed the worsening brain drain to poor funding, dilapidated infrastructure, harsh working conditions, insecurity, and weak policy implementation.
According to the General Medical Council of the United Kingdom, the number of Nigerian-trained doctors practising in the UK has climbed to 11,001.
The President of the Nigerian Medical Association, Prof. Bala Audu, recently warned that Nigeria has moved beyond passive brain drain and has become a direct recruitment hub for foreign governments seeking skilled medical professionals.
In an exclusive interview with PUNCH Healthwise, Audu revealed that international recruiters now visit Nigeria to directly hire doctors—particularly specialists such as obstetricians, gynaecologists, and paediatricians—offering them superior working conditions, remuneration, and infrastructure.
He lamented that while Nigeria’s population continues to grow and mortality rates remain high, the country is losing specialists at an alarming rate.
“Many of our doctors are not even going abroad to look for jobs. Foreign governments now come into Nigeria to pick doctors and take them away,” Audu said.
“We are still having more births, yet maternal deaths remain high because the skilled birth attendants who should care for these women are reducing every day.”
Audu added that in some specialties, the number of Nigerian doctors practising abroad may already exceed those still working within the country, a situation worsened by the government’s failure to significantly improve doctors’ welfare despite existing policy frameworks.
Experts have warned that with the current pace of emigration, it would be impossible for Nigeria to produce enough health workers to meet its growing healthcare demands. They estimate that it would take at least 20 years to train the over 400,000 health workers required to close the gap.
A former President of the NMA, Prof. Mike Ogirima, described Nigeria’s doctor-to-patient ratio as “horrible,” noting that the country currently has about one doctor to 8,000 patients—far below the World Health Organisation’s recommendation of one doctor to 600 patients.
In an earlier interview with PUNCH Healthwise, Ogirima said Nigeria produces an average of only 3,000 doctors annually, making it difficult to bridge the estimated deficit of nearly 300,000 doctors.
“If we are producing just 3,000 doctors yearly, it will take at least 10 years to catch up—and that is assuming no doctor leaves the system,” he said.
“We cannot afford to wait that long. That is why doctors are overworked, exhausted, and burned out.”
Ogirima urged the government to prioritise investment in health workers’ training, improve security, and provide modern equipment, warning that retention would remain difficult without adequate motivation and support.
Doctors have continued to call for urgent reforms to rescue Nigeria’s struggling healthcare system, stressing that a motivated and protected medical workforce is essential to national development.
They also urged federal and state governments to immediately enrol doctors in comprehensive insurance schemes as part of a broader welfare and retention strategy, warning that without decisive action, the crisis would continue to deepen.
Culled from The Punch