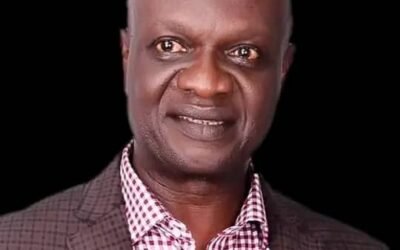
Nigeria’s former President, Dr. Goodluck Jonathan, will be one of the leading candidates to confront incumbent President Bola Tinubu, in the 2027 presidential poll, a close ally of the Bayelsa-born politician confirmed to Vanguard yesterday.
The ally, who is also in the People Democratic Party, PDP, as Jonathan, told Vanguard that the plan to draft the former President to contest on PDP’s platform had gone far, and that he had accepted, adding that the former president was going into the race to find ways of addressing Nigeria’s rising poverty, hardship and the general suffering that had gripped the citizenry in recent years.
The source said the project to bring back Jonathan to reposition Nigeria was being driven by key Nigerian leaders and elders, who believed the former president stabilised the country and its economy within the six years of his administration.
READ ALSO: CRSHA Member, SSG, Groups Eulogize Late Prof Ibiang Oden Ewa
The source said it was in a bid to rescue the country and restore the dwindling economy and Nigeria to its pride of place that key PDP leaders and elders started ‘pleading with him’ to consider running against Tinubu in 2027.
There are those who believe that giving him the opportunity to run for a single term of four years remained the clearest pathway for power to return to the north in 2031 and remain there for eight years without a serious struggle by the south.
Going by the fact that Jonathan had already served out a term of four years, he cannot run for more than another four years in office if he wins the election in 2027, just like Tinubu if he gets re-elected.
Jonathan’s ally said the Otuoke-born politician had already met behind the scene with some top leaders within and outside the PDP to consult them and seek their support for the 2027 presidential race.
According to the politician, Jonathan met with former Nigerian military president, General Ibrahim Babangida, retd., last weekend in his Hilltop Mansion in Minna, Niger State, and briefed him on his desire to run for one term in 2027.
Although the source did not say what General IBB’s response to Jonathan was, he, however, expressed optimism that the idea had been properly sold to the north.
The official also disclosed that Jonathan was currently in the South-South consulting and meeting with critical stakeholders, with a view to selling the project to them and soliciting their unflinching support.
It was, however, not clear at press time who the GEJ team was meeting with in Port Harcourt, the Rivers State capital on Tuesday and yesterday but it is believed that his support base in the region would not be a problem to him.